Remember – If you're enjoying these podcasts, please leave us a review in iTunes. Thanks!
Episode #80: The Hormone Cure with Dr. Sara Gottfried, pt 2
We hope you enjoyed last weeks podcast with Dr. Gottfried!
Check out Dr. Gottfried's website here.
Here is part 2 of our interview series with Dr. Sara Gottfried, hormone expert and author of The Hormone Cure!
We covered some more great topics in this episode including: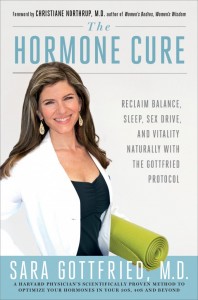
- Sex drive in early 20s?
- Birth control
- Fiber & foods for hormone balance
- Early menopause
Click here to download this episode as an MP3.
The episodes are currently available in iTunes, Stitcher & Blog Talk Radio.
LIZ WOLFE: Hey everyone, Liz and Diane here as usual. We are so thrilled to again have a special guest with us, Dr. Sara Gottfried, author of the new book, The Hormone Cure: Reclaim Balance, Sleep, Sex Drive, and Vitality Naturally with the Gottfried Protocol, which is officially a New York Times Bestseller. Woo hoo!
DIANE SANFILIPPO: Woo hoo!
SARA GOTTFRIED: Woo hoo!
LIZ WOLFE: I love that I know several people with books on the New York Times Bestseller list. That is…I hope some of that rubs off on me.
DIANE SANFILIPPO: Awesome.
LIZ WOLFE: That is amazing. Congratulations, Dr. Gottfried.
SARA GOTTFRIED: Thank you so much. I just feel thrilled that people are responding to the message and spreading the word. Thank you.
LIZ WOLFE: Yes. Well, if folks did not listen last week, please go back and listen to episode 79. We are absolutely in love with Dr…I'm going to call you Dr. Sara. [laughs] We're going to call you Dr. Hot actually. Dr. Hotfried.
SARA GOTTFRIED: Love it.
LIZ WOLFE: Love it. So we are absolutely in love with you. If you haven't gotten your hands on Dr. Gottfried's book yet, you must do so immediately. It's so dense in information and we're just so thrilled to have begged Dr. Hotfried on for a follow up show to answer a ton of your hormone related questions. Diane, do you have any opening notes?
DIANE SANFILIPPO: So Thursday, by the time this airs, I will be in Austin at PaleoFX, so just want to remind people, if you're there, come look for me.
LIZ WOLFE: Okay, well, perfect. We're doing a little less jibber jabber than we did in the last episode because folks have a ton of questions. Ready, Dr. Gottfried?
SARA GOTTFRIED: I'm ready. Let's do it.
LIZ WOLFE: All right, let's go for it. So we have a lot of questions about female hormones, birth control, libido, stuff like that, and the first question we'll start with is from Katie. She says: I'm 22, almost 23. Last May, right after I turned 22,my libido plummeted to the basement, which was very unfortunate since I got married in June. I've never been on artificial birth control. I use a Natural Family Planning/Fertility Awareness method; however, my mom was on the Pill before I was born, and throughout my childhood as was her mom before her. About the same time as my libido shot down, I got a yeast infection that has never completely gone away. I've been eating an almost vegetarian diet through my 4 years of college, mainly because the cafeteria meat was gross, but lots of commercial eggs. I drank coffee through college, but stopped ironically right before the libido drop. I stopped using commercial beauty products and began eating a Weston A. Price type, grain free diet last summer, including more meat, butter, fermented cod liver oil, raw dairy, etc. And I gave up all dairy at the end of January because it was making my menstrual cramps absolutely debilitating. Also, I've gained about 20 unwanted pounds. I was around 113 before my wedding in June, having lost about 10 pounds for the wedding, and I'm now around 133. I'm 5′ 2, and would be happy at 120 or so. And plenty of grass-fed meat, seafood, and veggies, high fat and protein, low carb. I haven't been eating eggs, though, because I think I may have developed some kind of reaction to them. They seem to make my joints swell. Sorry so complicated. My point is what am I doing wrong and how can I fix my libido so my patient and loving husband can enjoy every aspect of our marriage. Thanks so much.”
SARA GOTTFRIED: Hmm, well, first I want to say to Katie that, like many women who struggle with their libido, I think there's a tendency to blame yourself. And you know, when I hear in that final question, what am I doing wrong? I just want to say, it's not you, it's probably your hormones. We know that 70% of low sex drive, low libido, is hormonal. So let's start with the biology instead of, you know, deciding that you're doing something wrong. I just…I want to say that this is probably hormonal.
So let's unpack that for a moment. When I have a 22 year old, almost 23 year old, who's got low sex drive, definitely I think about birth control pills because that's the number one reason why libido is dropped. But that's not the situation here. She's described a number of different things. She also said she had a yeast infection that never went away, and so that makes me wonder if there's some issue with candida or if she has the right diagnosis. So I would want to make sure that she's seen a clinician, a nurse practitioner, or a doctor, who is making sure that she doesn't have either a hypersensitivity to yeast, and that can make sex painful, and who wants to have sex when your lady garden doesn't feel good.
LIZ WOLFE: [laughs]
SARA GOTTFRIED: So those things need to be addressed. I really think the yeast infection, you want to take that on. It certainly sounds to me like she is eating a very healthy diet, and so if I had someone in my practice with this situation, I would say, okay. Let's go back to those hormonal Charlie's Angels, and if you recall from last time, they are your cortisol, your estrogen, and your thyroid. And I wonder if Katie might have an issue with one or more of these three hormonal Charlie's Angels. And you got to remember that cortisol's the most important one here. it's the one that doctors are least likely to check. It's the main stress hormone, and it's also…it has this way of shutting down your other hormones. It can slow down your thyroid. It can block your progesterone receptor. You want to have this really good tango between estrogen and progesterone in order to really feel at home in your body, really feel like your sex drive is a match to maybe the love that you feel for your new husband.
So with those three hormones, cortisol, estrogen, thyroid, I would want to know, okay, where are you? Where are you? So there's a quiz that you can take. You can certainly read my book at the www.thehormonecurebook.com. You could also do a quiz. Can I mention the quiz?
LIZ WOLFE: Of course.
SARA GOTTFRIED: So this is a really good way to kind of see which of these hormonal Charlie's Angels is off. I take you through this self-assessment where you can figure out, okay, do I have one or more of the top 7 hormone imbalances that I've recognized in my practice over the past 10 years. So the quiz is www.thehormonecurebook.com/quiz. And hopefully you’ll have a URL that people can link on to get more information on that. But here's a couple of scenarios that I often see in someone who's 22, 23, and libido is plummeted. One is that cortisol's high. So high cortisol, that stress hormone, can really cause a lot of problems in the female body. And this is again, one of those things that your doctor is probably not going to check, but when cortisol's high, it depletes those happy brain chemicals, not just serotonin, like we talked about last time, which is in charge of mood, sleep, and appetite, but also dopamine. It can deplete dopamine. Dopamine is the neurotransmitter, the happy brain chemical in charge of pleasure and satisfaction. And I often find that dopamine is low in women who have low libido. So we want to take a look at cortisol. We want to look, you know, the way I look at this is you want to look upstream from whatever hormones are out of whack to ask why. Okay, what's the root cause? If the root cause of your low libido is high cortisol, what's going on? Is it something to do with your work? Is it an allergy to some of the foods that you're eating? Is that raising your cortisol level? We know it can do that. Sometimes just going to a food plan that is very low in carbohydrates can actually cause some of your hormones to be off. Sometimes raise your cortisol. You need to have some carbohydrates. It can also slow down your thyroid.
So now we're going to bring in another Angel. So your thyroid, you know, a lot of people think thyroid is that hormone that can be off when you're older. And the truth is, many things can cause problems with your thyroid. When I was in my 30s, high cortisol was slowing down my thyroid, and it was making me fat, cranky, and tired. And who wants to have sex when you feel fat, cranky, and tired? So I would say, let's look at those three hormoneSara Gottfried: cortisol, estrogen, and thyroid. We want to especially look at the balance, progesterone. I'll give you a little tip here from my book. You want to have a progesterone to estrodiol ratio. Estrodiol is one of your estrogen hormones. You have to have a ratio of about 300, so that means 300 times more progesterone to estrodiol when you're around day 21 of your menstrual cycle. That's for a 28 day cycle. So I have to tell you, you know, when I was on last time, you guys told me, Liz and Diane, that I could go into a little more biochemistry. So I hope this is coming across well, but the idea here with that tango between estrogen and progesterone, the one that really makes you love up your husband and want to have sex, is that you have 300 times more progesterone to estrogen molecules. So short version. Check those three hormonal Charlie's Angels. And then another, a 4th hormone you want to check out is testosterone.
LIZ WOLFE: So a quick follow up question to that, Dr. Gottfried. This is Liz. So it's not, like you keep saying, a lot of this stuff that's happening, is happening to people in their twenties, when they're really young with loss of libido, maybe compromised thyroid function. These things that we associate with aging, you're actually seeing this in younger people on a regular basis?
SARA GOTTFRIED: Definitely. Definitely. And I think there's a few reasons for that. I think we're, as women, we're more stressed now than ever before in the history of the world. I mean, sad to say, some of us are able to roll with the punches, but I would say, many of us are in that situation that I was in in my thirties, where I was not rolling with the punches, let's just put it that way. My cortisol was 3 times what it should have been in the morning in my blood.
LIZ WOLFE: Wow.
SARA GOTTFRIED: And it gave me, you know, that muffin top. It depleted my happy brain chemicals, and I blamed my husband for pretty much all the misery in my life. So that wasn't very effective. [laughs] And it made my PMS worse. It gave me some mild Polycystic Ovarian Syndrome symptoms, and I definitely see this happening younger and younger. So there’s, number one, the increased stress, this connectivity, this, you know, sort of constantly available, hurry up lifestyle that we're all existing in, which is a double-edged sword. Like there's some beautiful aspects to it, but it's also…it's hard to manage. It's hard to turn it off.
LIZ WOLFE: Mm-hmm.
SARA GOTTFRIED: Second issue is endocrine disruptors, and I don't want to get on a soapbox about it, but I definitely think that we have all of these chemicals in the environment. More than 700 that bind to the estrogen receptor. Many also bind to the thyroid receptor. Whether that's your living room couch or your mattress or the food that you're eating, you definitely are getting exposed to these endocrine disruptors and they can rob us of sex drive. They can rob us of ease around our weight. They can undermine your weight loss. You know, there was just a study…I'll just mention a quick study here, especially related to Katie and her question about weight gain. Endocrine disruptors are…if you just look at thyroid disruptors for a moment, there's just a study looking at, if you lose weight, if you lose 10 to 20 pounds, what happens when you lose weight is you start to burn fat and some of that fat actually is storing these endocrine disruptors. So you may have walled off, kind of imprisoned the endocrine disruptors in your body, and then the terrible irony is that when you lose weight, when you lose 10 or 20 pounds, those endocrine disruptors get out of jail.
LIZ WOLFE: Yup.
SARA GOTTFRIED: And they start to bind your receptors, slow down your thyroid and make it even harder to lose weight. You can even gain weight as a result of this. So it's an unfortunate catch-22 that we want to be aware of.
LIZ WOLFE: And would you say that that's kind of like a detox, kind of that detox effect? Maybe that people feel or observe, you know, these maybe even wilder, feeling hormonal type swings when they're actually trying to do something good and recover from these things?
SARA GOTTFRIED: Yeah, I would say it's a detox effect. I mean, I think about detox effects as being the symptoms of getting off of caffeine, or the symptoms of, you know, trying to get alcohol out of your system, and how that can make you actually feel miserable for awhile, even though you're doing the right thing for your body. So the detox…I think we could qualify this as a detox symptom. You know, what just makes my heart sink is that when people are doing the right thing, when they're trying to detox, when they're trying to lose weight, when they're trying to create more of a nourishing relationship with the food that they're eating, it just makes me crazy that they're undermined by this endocrine disruptors. So we've got to do our best to reduce exposure and then to try to get these out of our system.
DIANE SANFILIPPO: Is this the type of situation where you might call for some supplemental support? Something like milk thistle or silymarin or something for liver detox or like diindolylmethane. Is that supportive here? Or not really that helpful?
SARA GOTTFRIED: Oh definitely. So I think there's certain supplements that are very effective when it comes to detoxing and getting endocrine disruptors out of your system. I am very data driven. I don't know if you noticed, but I'm very…I'm a bit of a geek when it comes to these things. So we know with milk thistle, for instance, it's a great way to love up your liver. So I'm a huge fan of milk thistle as a way of helping your liver process all of these hormones and endocrine disruptors that it's coming up against. And we know that as you get older, like when you're starting in your 30s, your liver doesn't do quite the same job that it did when you were a teenager or in your 20s. You know, it's not like a fine Bordeaux that gets better with time. We want to do everything we can to take care of the liver. So yes, milk thistle I think is very effective. I also would put in a huge plug for fiber. You know, the same mechanisms in your body that process estrogen also process these endocrine disruptors. And so we've got to be really careful about making sure that the liver is clean and operating at peak performance. And I think both milk thistle and fiber do that. I also think we tend to run out of certain amino acids, and we have to fill that tank. That's one of the reasons why I love a diet that is a little richer in protein, so that you're getting sufficient protein, especially when you want to detox.
DIANE SANFILIPPO: This is a random, maybe it's a poop question. I'm known for being the one who talks about poop a lot. Is fiber supportive and helpful because we're actually detoxing a lot of this stuff through our stool, our eliminations? Is that why fiber is supportive?
SARA GOTTFRIED: Yeah, fiber's supportive for a couple of reasons. The whole idea with estrogen, you know, if we just take on estrogen, for a moment, one of those hormonal Charlie's Angels. The idea with estrogen is you want to find that Goldilocks position of not too high, not too low when it comes to estrogen. You want it to be in that tango with progesterone. You want to have, as I mentioned, with this ratio, you want to have about 300 times more progesterone to estrogen when you're cycling around on day 21. And if you have too much of it, that can cause a number of symptoms. It can give you low libido, like Katie was describing. It can make it very difficult to lose weight. It can make you have breast tenderness. It can make your periods more painful. There's a long list. Autoimmune conditions. It can cause issues with your joints. You know, as I say that, I'm thinking about how Katie had many of these symptoms.
LIZ WOLFE: Mm-hmm.
SARA GOTTFRIED: When you have fiber, when you have sufficient fiber, I think we should have the fiber talk now. So when you have [laughs]
LIZ WOLFE: [laughs]
SARA GOTTFRIED: So with fiber, here’s the deal. We know that the average American woman gets about 13 grams, 14 grams of fiber a day. And that is a pitiful amount. You need to get about 45 grams a day, even 50 grams, to really be able to get rid of the stuff you need to get rid of. Excrete the bad stuff, and keep the good stuff. So fiber does a couple of things. It allows you to use estrogen and then lose it. You got to use it and then lose it. You don't want to keep recycling it. This is one situation where recycling is not a good idea. So you want to use it and then you want to poop it out with the fiber. You also pee it out. Those are good things. The other thing that fiber does is it helps you get the right balance of bacteria in your gut. It helps you with having biodiversity among those lovely bugs that are your BFFs in your gut. So fiber has many important functions. Those are a couple of them.
LIZ WOLFE: And would that be a mix of soluble and insoluble fiber? from you know, leafy greens and what…like the inside of the sweet potato for soluble fiber?
SARA GOTTFRIED: Yes, absolutely. I'm a big fan of getting fiber, mostly from food, although I have to tell you. Even when I'm eating like a rock star, the best I can do with food is typically around 25, maybe 30 grams a day. And that's with 7 servings of fresh vegetables. I don't eat much fruit. But that's with 7 servings of vegetables a day and getting fiber wherever I can. So I need supplemental fiber. Soluble/insoluble mix. You know, what a lot of people start with is a 50/50 mix and then they sort of see what happens with their bowel function. And I'm right there with you. I love to talk about pooping. I think it's a really important thing to be discussing, and we know if your thyroid's not working, there's a good chance that you're going to be a little slower…
LIZ WOLFE: Sure.
SARA GOTTFRIED: to get your food through your system, extract the nutrients you need, and then have it come out the other end. So what’s normal is for the transit time, from when you eat that sweet potato to when it comes out on the other end is about 12 to 24 hours. So if you're not pooping once or twice a day, I consider that to be constipation. We need to look further. But in terms of figuring out that blend of soluble vs. insoluble, I find that everyone's a little different. You know that old school medicine idea, one size fits all, blanket statement of what everyone needs in terms of soluble vs. insoluble, I don't believe in that so much. So I usually suggest, start with 50/50, and then make adjustments so that you've got this transit time of 12 to 24 hours. But I want to hear what you guys have to say about this too because you know a lot about fiber and transit time.
DIANE SANFILIPPO: Well, it's funny that you mention the different balances and all of that. When Liz and I were at the Charles Poliquin certification over the summer, I think it was, last summer or felt like summer because we were in Arizona.
LIZ WOLFE: We were in Arizona.
DIANE SANFILIPPO: When was it? I don't even know.
LIZ WOLFE: Not a clue.
DIANE SANFILIPPO: But I remember they were talking about hormone detox and fiber was a really big point then. And it's something that when we're talking most just about digestive function, we actually, or at least I like to sort of bust the myth that we need tons and tons of fiber to actually go to the bathroom because…
LIZ WOLFE: From whole grains.
DIANE SANFILIPPO: Yeah, just from grains because there's, you know, 100 people in the room that we're teaching who don't eat grains and who poop once or twice a day. So we're like, we don't need to get it that way necessarily, but we do talk about the difference between the insoluble and the soluble and how a lot of people that we're talking to have so many digestive issues that too much of the insoluble, too much of the leafy greens and other kind of more irritating sweeping fibers vs. the ones that do a little more to feed the bacteria, the soluble fiber. You know, we tend to recommend of the soluble than the insoluble for that reason. But I think that this is a good point because it is a different situation and it's a different issue that some women are dealing with, and if they're not having trouble going to the bathroom or they're, you know, feeling like they digest leafy greens and all other types of vegetables just fine, then this is something that, you know, could definitely be a step for them. I know, I don't really digest things like kale that well. If I eat kale, I tend to see a little bit too much of it, you know, not completely broken down when I go to the bathroom, and I know it's not a good situation for me. But I think it's important to point out that these are different, just variations on times to really consider that in a different approach. And I do want to point out, too. You mentioned transit time, and I have a transit time test in my book on the Guide to Digestion, and it's swallowing, well, you have to kind of take them with a little bit of water, two, I think it's two tablespoons of white sesame seeds, so they're, you know, it takes a little swig of water to get them down after a meal. And then seeing when the bulk of them come out in the toilet, and that will tell you how long it took that one meal to go through. So for people who are wondering how to actually test that, you can do it that way at home.
SARA GOTTFRIED: That's great. That's great. It sounds like you and I are doing similar things in the bathroom. [laughs]
DIANE SANFILIPPO: With the Squatty Potty? Do you have a Squatty Potty?
SARA GOTTFRIED: Oh yes! Got to get the angles right.
LIZ WOLFE: You guys, I want to be in this poop party! Serious.
DIANE SANFILIPPO: I've got like wicker boxes. I'll just kind of store toilet paper in, and then pull it in front of the toilet and yeah.
SARA GOTTFRIED: Whatever it takes. By any means necessary.
DIANE SANFILIPPO: Exactly.
LIZ WOLFE: All right, I got to make a t-shirt or something. I'm invited to the poop party.
DIANE SANFILIPPO: Yeah.
LIZ WOLFE: I want to be cool, too. All right.
SARA GOTTFRIED: We need to rebrand pooping. Let's just put it out there. We need to rebrand hormones, we need to rebrand pooping.
LIZ WOLFE: Yes!
DIANE SANFILIPPO: Well, the Poop Pageant in my book has been pretty popular, just, you know, people want to have that Miss Ideal in their toilet. It sounds terrible. Oh goodness. Anyway.
LIZ WOLFE: I just like all of the alliteration, as someone who's originally an English major. Poop Pageant. Poop Party. Like it.
DIANE SANFILIPPO: That’s right.
LIZ WOLFE: All right. And the assonance. Squatty Potty. I like that, too. All right, so moving right along. This next question is from Lauren. “What advice can Dr. Gottfried give for women coming off long term Depo progesterone only contraception. Quit 15 months ago, but was on for 18 months. According to a salivary panel, my estrogen levels are extremely low. Testosterone is very high. Progesterone appears normal. Melatonin is too high at night and upon waking. Cortisol is relatively low upon waking, peaks at mid-day, then stays elevated until late evening. How can I go about the complex issue of rebalancing my hormones beyond just following a strict Paleo diet?”
SARA GOTTFRIED: Okay, Lauren. Well, as you know, I can't give medical advice. I have to do a full history and physical to give medical advice, but I can tell you how I would approach this for someone who's in my medical practice. It turns out that, as you might be able to tell from the way I talk about synthetic hormones, I'm not a big fan of Depo-Provera, and for those who don't know what that is, it's a basically this large dose of synthetic progestin which is injected into your body and it lasts for about 3 months, and it keeps you from getting pregnant. I'm not a fan of it because I just don't think synthetic hormones have a time and a place inside the female body unless you're in extreme situation like endometriosis and the alternative is surgery. So I'm not a big fan of synthetic hormones. And as Lauren is describing, I think very articulately, she's having some long term consequences from having these synthetic hormones in her body. We know they can last in your body for years. You know, it can take that long to detox. We were just talking about how estrogen can, you know, get stored in your fat cells, and when you lose weight, for instance, some of it can get released. So these things can get stored in your body for a very long time.
So let's just take some of these issues that she's raised. I like to be really systematic about approaching these so that it's not confusing. So let's go back to the hormonal Charlie's Angels. I feel like we can all chant them together now. So they are cortisol, estrogen, and thyroid. I haven't heard anything about thyroid here. But looking at some of these other Charlie's Angels, she said that her estrogen's very low and her progesterone is normal. Do we know Lauren's age? I assume she's probably like 20s, 30s, something like that.
LIZ WOLFE: We don't have it, unfortunately.
SARA GOTTFRIED: Okay. Okay, so what we know is that your estrogen and progesterone can start to change as early as 28, even without being on any synthetic hormones or contraception. So you can start to drop your estrogen a little bit, you know, in your late 20s. It's usually not much of a shift until you get to somewhere in that window of 35 to 45, but having such a low estrogen makes me wonder about whether the Depo-Provera is actually doing that. So what are some of the ways that you can actually raise your estrogen naturally? She mentioned that her progesterone looks normal, so I assume what she's saying is, that the ratio between estrogen and progesterone, I just mentioned you want that ratio of progesterone divided by estrodiol. You have to make sure they're in the same units. Be a little geeky here about the math. You want that ratio to be about 300. So let's just talk about low estrogen for a moment, and in my book, in Chapter 7, I talk quite a bit about low estrogen. I don't think Lauren described her symptoms, but I can tell you, for women who have low estrogen, especially before menopause, typically what they feel are mood issues. You know, I know that 20 to 30 percent of women are very sensitive to estrogen levels, and it can make them feel mildly depressed when estrogen is low. It can also cause issues with getting pregnant. It can make you have trouble with breastfeeding. When estrogen's too low, and then breastfeeding further suppresses it. It can make you feel less juicy, so you can have vaginal dryness, sex can be painful, your joints can be less juicy. So you may be more prone to injury.
So what are some of the things that actually help you with low estrogen? I would start with step 1 of the Gottfried Protocol, which is those targeted lifestyle changes and filling nutritional gaps. This is where we know that avoiding coffee is really important. So we know that caffeine and coffee have been shown to lower estrogen levels in women who are pre-menopausal. It sounds like Lauren is already avoiding gluten, but gluten can also cause a problem with your ovaries, and so I really encourage women with low estrogen to just avoid gluten completely. So one of my favorite ways to raise your estrogen level is actually orgasm. I said it again. So orgasm, you know, where your body gets flooded with oxytocin is one of the most powerful ways to work with some of these hormone issues that she has. It balances out your cortisol. It also helps to raise your estrodiol. So I think that would be a really good solution for her and I think we even talked last time about orgasmic meditation.
A couple of other things. Magnesium has actually been shown to be helpful. It helps with the symptoms of low estrogen. Vitamin E. Those are some of the step one solutions. Step 2 is proven botanicals. I'll just give you one example here: Maca. I love me some Maca. And then last, I would say for her, taking on the cortisol, it sounds like she's got a disrupted curve when it comes to her cortisol levels, and I think what we should do is maybe just talk for a moment about cortisol, kind of what's normal in terms of the levels, so that we can generalize this for others. How does that sound?
LIZ WOLFE: Sounds good to me.
SARA GOTTFRIED: Cool. Okay, so here's the deal with cortisol. It’s not just a flat line all day long. What you want with cortisol is a peak level in that Goldilocks’ position of not too high, not too low, a peak level within an hour of getting up in the morning. And then you want this nice little downhill ski slope over the course of the day, where your lowest level is before you go to bed. And what we're hearing from Lauren is that she's actually low in the morning, she has this little period where it's normal during the day, and then she's high at night. So she has what's called a reverse curve or an inverted curve where she's low in the morning and high at night, and that tends to give you a second wind. It tends to make it hard to unwind at night and it also tends to make women feel hyperviligilant. Like it's just really hard to kind of turn off that constant mental chatter, the monkey mind.
One of the things that I think is really effective to do here, what I would suggest to someone in my practice, is to take on that cortisol. You got to get it so that it’s serving you and not working against you. It is the most important hormonal Charlie's Angels here. And what I would suggest to start with, just like a simple solution would be to do some form of exercise that helps you get into the normal range with your cortisol first thing in the morning. So if this was my curve, for instance, I would say, honey, you should go running or go to, you know, like a Zumba class in the morning. That would help you get your cortisol into the normal level first thing in the morning, and then at night, I actually did this with a woman I saw this week. A woman named Joanie, who is a 38 year old woman with high cortisol at night. We made one change. I gave her something called Cortisol Manager. Cortisol Manager. And this really helped her turn off the lights at night. So she was able to get her cortisol into the normal range, just by taking Cortisol Manager. You just follow the directions. It's available online. Cortisol Manager, very effective. It's a combination of ashwaganda and also a few other elements that help you get that cortisol into the normal range.
DIANE SANFILIPPO: Yeah, this looks like some…I'm actually looking at it now. Ashwaganda, phosphatidylserine, some adaptogens, I guess on the PS. Yeah. For sure. I actually just had a really quick question. I don't know if you've seen this before. Women who have that sort of tired and wired cortisol going on, but if they exercise in the morning or any like early part of the day, say before noon, it leaves them feeling even more flattened out after that. Have you seen that happen?
SARA GOTTFRIED: Oh, definitely. Definitely. So the idea here is we're trying to find that neutralized place with cortisol where it's able to do its job in your body and it's not working against you. And what I see is a lot of people who have that tired but wired feeling, they're actually high on cortisol. That's the typical situation. Cortisol's a little sneaky and you can't always gauge exactly what's going on with it, but people who've got that paradoxical combination of tired but wired, typically they have high cortisol. If you have high cortisol, going running or going to a Zumba class is the worst possible thing because that depletes you further. It raises your cortisol even more. Now for people who are runners and they just can't imagine life without running in the morning, one thing you can do is you can take vitamin C, and that's been shown to blunt that cortisol effect. So you'll be a little better off if you take about 750 to 1000 milligrams of vitamin C before you go running. But what I recommend instead is that you're exercising smarter, not harder. And in this situation when you're tired but wired, maybe have high cortisol in the morning, I'm a big fan of adaptive exercise. And by that I mean, go to Pilates. Go to a yoga class. Do a DVD at home for a barre workout. You know, there's lots of different ways that you can do this where you're not going to deplete yourself and then feel even worse. The other point that I want to raise here for people who are tired but wired, there's a deeper issue of mitochondrial fatigue. There, I said it. Should we talk about mitochondrial fatigue for a moment?
LIZ WOLFE: Yes.
DIANE SANFILIPPO: Yes, please indulge me because I'm pretty sure that's what my body's doing right now, so please.
SARA GOTTFRIED: Okay. All right, well, your mitochondria are these super cute little power factories that you have in each of your cells. They're super important. And what happens is, many of us have a tendency to burn the candle at both ends. I don't know if you can relate to that at all, Diane and Liz.
LIZ WOLFE: Hahahahaha.
DIANE SANFILIPPO: Not at all.
SARA GOTTFRIED: No, I didn't think so. Me neither. So when you're someone who, you know, has…is mission driven, and you've got like a big vision for what you want in the world, I think you're especially vulnerable to mitochondrial fatigue. And that's where these cute little power factories just start running out of sauce. Like they don’t have enough power coming in to keep up with the output. So we want to have a little more input than output, right? I mean, we want to be running at a net positive when it comes to our energy and our power. And we want to be thinking of all the ways that we can be doing that globally, but then taking it down to the mitochondria, there's a couple of ways that you can help this problem. So if you especially feel depleted after exercise, I think about cortisol and you know, getting the right match with exercise, and then I also think about mitochondrial fatigue. What's been proven to make a difference is UBQH, UBQH, ubiquinol, which is the active form of CoQ10, that's been shown to be really helpful. D-ribose has been helpful. So these are some of the solutions that you can try. I’m also a big fan of resveratrol. That's kind of the trio that I think about with mitochondrial fatigue. UBQH, d-ribose, and resveratrol.
DIANE SANFILIPPO: Stocking up.
SARA GOTTFRIED: Stocking up. Ordering now.
LIZ WOLFE: Let's, if it's okay, guys, switch gears real quick, for just kind of a really common, really quick question. [laughs] I hope as many people are as interested in this question as I am. If not, I apologize. Okay, Carol asks, “is hair around the nipple common or normal for women, or is this caused by a hormonal imbalance? I'm not talking about a lot of hair, but maybe 5 follicles or so that continuously grow despite regularly removing them? Thanks.”
SARA GOTTFRIED: Hmm. Well, you thought this was simple and quick.
LIZ WOLFE: Uh oh.
SARA GOTTFRIED: Let's see. It's a little hard for me to say whether something is completely normal or not without doing a full history and exam. 5 follicles, I don't get super excited about that. I mean, I can tell you from being board certified in everything that can go wrong with the female body, that's not an outlier. That's not something that makes me really worried. I've looked at a lot of women's bodies, done a lot of exams, about 20, 000 in the past 20 years and overall, I can say that I'm not too concerned about that. But for women who are distressed by it, who feel like, okay, it's 5, a month later it's 10, and now I'm seeing them on my chinny-chin-chin. Like those women, I would want to go see your clinician and get diagnosed. Get your hormones tested. See if you have something like polycystic ovarian syndrome or if there's some reason why you're making too much testosterone. So those are some of the things I think of. There's also many, many, many women who have a family predisposition to have 5 hairs on their nipple. So, you know, I'm not too concerned about it. It just sort of depends on your context. It depends on…is this worsening? Are you distressed about it? Is the rest of your family a little hairy?
LIZ WOLFE: Got it. And to that…to that answer, we have another question about balancing PCOS. Is it possible to balance PCOS without the use of birth control pills and metformin? That's from April.
SARA GOTTFRIED: Absolutely. Have faith. So I have an entire chapter on this, it's chapter 8 in my book, The Hormone Cure, and the idea here is that we live in a culture that is so prescription happy. And I was trained to do this, right? I'm not blaming conventional doctors for this, but what I found was that I was trained to diagnose polycystic ovarian syndrome, and then immediately go to birth control pills, metformin, and the like. When I realized that you could actually balance your hormones naturally with how you eat, move, think, and supplement, and then I took on PCOS for this chapter in the book, I was delighted to see incredible solutions that are out there that are completely natural and by the way, are more effective than metformin. So let me give you a few examples of this. And with PCOS, that's something that you do want diagnosed with your clinician. You don't want to just rely on me talking about it. I can't give you medical advice. But here's what been shown to make a difference. Gottfried Protocol step 1, those targeted lifestyle changes and nutraceuticals. We know that when you reduce your glycemic index, within 7 days, that can lower your testosterone levels by 20%. I think we talked about that last time. We also know that exercise is really effective. The cool part here for women who are a little overweight or obese wit polycystic ovarian syndrome, even a 5 to 10% change in your weight can reverse the chemistry, the altered chemistry of PCOS. There's another situation where fiber makes a big difference. Can’t say enough about fiber. Zinc is also incredibly important. We know zinc is really crucial for that hormonal Charlie’s Angel, thyroid. It's also important when it comes to high testosterone and what has zinc…here's a few food sources. I'm a big fan of green beans. Here's those sesame seeds again. Here you get two for one. You get to do the transit time with your gut and then you also get to lower your testosterone levels.
DIANE SANFILIPPO: [laughs]
SARA GOTTFRIED: Pumpkin seeds also are rich in zinc. You want to avoid dairy. If you're eating Paleo, you probably have all these covered. You want to eat more protein, omit sugar. Get your oil changed.
DIANE SANFILIPPO: Oysters, too.
SARA GOTTFRIED: What's that?
DIANE SANFILIPPO: The zinc, too.
LIZ WOLFE: Diane loves oysters.
SARA GOTTFRIED: Oh, oysters, yes. Absolutely. And some of the insulin sensitizers. So let me back up for a minute. Metformin helps your cells become more sensitive to insulin. The idea with polycystic ovarian syndrome is that somewhere around 70% of people with polycystic ovarian syndrome are insulin resistant. So their cells are numb to insulin. Metformin is a prescription drug that helps you become more sensitive to insulin again, so you're less likely to just lay down fat, you know, when you look at a piece of chocolate cake. So the idea here is we want some natural alternatives to metformin that are also effective. Here's some of them. Chromium. Chromium's super effective. Inositol. Inositol is a form of a B vitamin, and we know that it improves insulin sensitivity. There's many studies showing this. There's a couple different types of inositol. There's d-chiro-inositol and myo-inositol. I talk about these in my book, page 227. Vitamin D also super effective, and then Gottfried Protocol step 2, we know that cinnamon is super helpful. So is saw palmetto and last thing I'll mention here is a really interesting formulation from Chinese medicine and I don't even know how to pronounce this. I’m going to butcher it, I'm sure, but it's Tian Gui. I'll spell it: T-I-A-N, next word, G-U-I. And this particular formulation has been shown to be more effective than metformin at lowering androgens and reversing PCOS.
DIANE SANFILIPPO: Awesome. It's great to hear you say all of that. A lot of the answers we've given to women asking about PCOS, kind of the first step we give them is to reduce sugar intake, and that doesn't mean a no carb diet, it just means really cutting back so that their insulin can get under control, get the rest of their hormones under control, as you mentioned, testosterone. In my Sugar Detox program, I recommend a bunch of supplements that are just, you know, additional support that people can use or don't have to, and chromium and cinnamon are high on that list, so it’s good to hear you say that, and it's reinforcing, for sure.
SARA GOTTFRIED: Yes, we are all in the same page. I would even say that the food plan that you guys talk about at Balanced Bites, I believe it can reverse insulin resistance in 48 hours. You know, if you really put in a huge effort and you really do it right. This is not some gigantic project that's going to take months and months. You can reverse this in 48 hours.
DIANE SANFILIPPO: It's staggering, and I'm not really saying anything that's so new, right? It's just maybe putting it in some language that's easy for people to understand, but it is pretty staggering and I'm so glad that we're all kind of out there reaching more and more people with the information in our book, so I'm just thrilled that your book is approaching it from this hormone perspective because it's probably…Liz, would you say at least 50% of the questions we get on the podcast are sort of female hormone related?
LIZ WOLFE: Yeah, at this point, definitely.
DIANE SANFILIPPO: I feel like there needs to be a television show about this.
SARA GOTTFRIED: Oh.
DIANE SANFILIPPO: If you're interested in a TV show, Dr. Gottfried, I think that would be a good idea.
SARA GOTTFRIED: Let's do it. And I would say it's not just that you put this information together in a particular way, it's that you allow people to have fun while they're
doing this, and the fun factor is essential. I mean, who wants to balance their hormones if it is torture? No.
DIANE SANFILIPPO: It doesn't taste good, right? It has to taste good.
SARA GOTTFRIED: It doesn't taste good. No, you want to have fun, you want it to taste good. We got to have more pleasure in our lives, right? And stop pushing the rock up the hill.
DIANE SANFILIPPO: For sure. I'm excited, too, because next week at PaleoFX I'll be on a panel about women's health, so I'll be sure to kind of name drop you and mention your book if the time comes.
LIZ WOLFE: And if you're ever bored, Dr. Gottfried, please just Skype us and we'll record an impromptu podcast because we have…I'm just looking at this Facebook string of questions. We have so many questions, and like you said, and like we'll, you know, append the beginning of our podcast, you can't give medical advice. None of this is direct medical advice, so you know, take everything that we're saying as information to, you know, inform your path going forward. But definitely you know, consult with your clinician and do and definitely get Dr. Gottfried's book to help you out if you submitted these questions because again that book is so dense in information with all of the different questions we've got through Facebook and the ones we're not going to be able to get to, the answer is probably in there.
DIANE SANFILIPPO: I think one of the things that women will end up realizing, which you and I, Liz, we're like broken records. We're always telling women to be a little bit more patient with themselves, to kind of slow down and, you know, we have to tell it to ourselves as well, I think.
LIZ WOLFE: Mm-hmm.
DIANE SANFILIPPO: But I almost think that when you sit down to read these things and you realize just how much you're pushing yourself without just, you know, paying attention to it and being a little bit kinder and just relaxing a little bit more. I'm talking to myself right now obviously. So…
LIZ WOLFE: Dr. Gottfried, do you have time for one more question?
SARA GOTTFRIED: Sure, let's do one more.
LIZ WOLFE: Thank you so much. Okay, this one is about early menopause. This is from Facebook. “I was diagnosed with early menopause in June of 2012 after having a Mirena removed in March of the same year. I had the IUD removed because I had horrible hot flashes, night sweats, mood swings, acne, weight gain, lethargy, breakthrough bleeding, etc. I've had every test possible to confirm this, blood tests, saliva, and even an MRI. Been Paleo for about 4 years, not sure if I'm genetically predisposed to this because no other women in my family experienced this. I tried some low dose hormones to try and help with symptoms for a bit, also on a few supplements. Not sure if my hormones are just really messed up from almost ten years of Mirena or should I just accept that I'm going to go through the change early?”
SARA GOTTFRIED: Hmm. Well, again, I don't know all the labs to be able to comment on this in a rigorous way, but let me just say some general things about what I would tell someone in my practice. First of all, I would never accept some sort of dismal fate. In fact, I call…what I would call the situation is instead of early menopause, I would call it, the technical term would be premature ovarian insufficiency. With the idea being that maybe we could jumpstart your ovaries, and I wouldn't give up the faith on that. So you've heard me rant already about synthetic hormones and how I don't think they're a good thing for the female body unless you know, the alternative is surgery. So I'm not a big fan of the Mirena. I've had a Mirena myself, and I actually found that it decreased my sex drive, and I definitely see in 10 to 20% of my clients that when they're on the Mirena or some other form of IUD, which is releasing synthetic hormones, that it affects their whole body. You know, the idea that the makers of Mirena want you to believe is that it's synthetic progestin that's only released in your uterus, and I just want to bust that myth right now because it's released elsewhere in your body. So I don't know if the Mirena was related to the symptoms that this woman is having of low estrogen, but I suspect it is. It certainly sounds like a curious time frame. And all that we discussed before with the woman who came off the Depo-Provera, you know, these two situations are very similar. Both of them have low estrogen, so the same Gottfried Protocol applies here. You heard me talk about when you have low estrogen, step 1 of the Gottfried Protocol, those targeted lifestyle changes. You're avoiding coffee, you're cutting out gluten. This is one situation where acupuncture has been shown to be incredibly effective. Maca is one of my favorite solutions. You want to be cutting out gluten, sounds like you're doing that already because gluten can actually cause premature ovarian insufficiency. It can cause low estrogen. So I'm glad that you're following the food plan that we're talking about here today because it's very effective. And then what I would say is keep the faith. Keep the faith. You know what, if you haven't tried acupuncture, I think that would be a really good thing to work with. I think you also want to be looking at these other hormonal Charlie's Angels, so the tendency, what I was trained to do as a gynecologist, when you see someone who's got hot flashes and nigtsweats and symptoms of menopause and they're young, the tendency is just to look at estrogen and progesterone. But I would say, let's broaden the view. Let's look at those hormonal Charlie's Angels, cortisol, estrogen, and thyroid. What's going on with your cortisol? What's going on with your thyroid? So with someone in my practice, I'd want to look at that whole package, and also get you started on some of these natural solutions that can help you get your ovaries to work for you again.
LIZ WOLFE: The diagnosis is not a life sentence. Many diagnoses, in fact, are not, you know, patience and persistence, and the Gottfried Protocol.
SARA GOTTFRIED: That's right. And you know, if you learn nothing else today, I want you to understand that it's easier to rebalance your hormones than to live with the misery of hormone imbalance. I think that's a really important message. You know, we're not talking about a gigantic project. We're just talking about a few steps that can really get you feeling full up. You know, back in your body again and feeling like you can rock your mission.
LIZ WOLFE: I love it. Rock your mission. Well, we'll close out with that. That's it. Huge thank you to Dr. Gottfried for being with us once again. I can't say enough great things about her book. It's called The Hormone Cure: Reclaim Balance, Sleep, Sex Drive, and Vitality Naturally with the Gottfried Protocol. It's officially a New York Times Bestseller. Go order it now. As usual, you can find Diane at www.blog.balancedbites.com. You can find me, Liz, at www.cavegirleats.com. And you can find Dr. Gottfried, I believe there are two websites, www.saragottfriedmd.com. We also talked about www.thehormonecurebook.com. Did I get all of them, Dr. Gottfried?
SARA GOTTFRIED: You totally did. You know, I always have to say Sara without an H, Gottfried, like fried, and so I just did www.thehormonecurebook.com to keep it easier.
DIANE SANFILIPPO: Yeah, we'll link to all of them in the show notes.
SARA GOTTFRIED: Thank you.
LIZ WOLFE: Perfect, well again, thank you so much, Dr. Gottfried for being with us.
SARA GOTTFRIED: My pleasure. Thank you so much.
LIZ WOLFE: And thanks everyone for listening. We will be back next week.
Cheers!
Diane & Liz


Comments 13
There is no link to listen…only mp3.
Yes, that’s how the click here always works – you can go to http://blogtalkradio.com/balancedbites anytime as well.
I love love love you guys, but I don’t know how I feel about the new intro…it doesn’t seem to fit your vibe. Great podcasts with Dr. Sara. Love your content and use my signed copy of Practical Paleo all the time! Looking forward to more great podcasts.
We’re trying to spruce up our previously uber-casual vibe just a touch with something standardized each week for an intro- thanks though! 🙂
Another great episode gals! I love it when Dr. Sara gets into the science. As a Midwife and health professional I love learning about all the physiology of what’s going on in our bodies. Just picked up the book and now have some great easter reading to do!
Awesome, awesome set of podcasts! I hope you have her back on the show because she made the information so clear and accessible. I’m so glad you had her back for a second.
I was curious about something that she mentioned–she said that low estrogen can cause difficulties with breastfeeding. I am an IBCLC (International Board Certified Lactation Consultant) in private practice in NYC and the research on breastfeeding hormones that I’ve seen indicates that estrogen does not play a critical role at all. Breastfeeding: A Guide for the Medical Profession by Ruth Lawrence says this: “A complex sequence of events, governed by hormonal action, prepares the breast for lactation. 17β-Estradiol stimulates the ductal system of epithelial cells to elongate during pregnancy. In contrast to puberty, however, when estrogens appear to directly and indirectly stimulate breast development, estrogens have no indispensable role in mammary development during pregnancy except as a prolactin potentiator: according to Neville, when estrogen levels are low in pregnancy, the breast still develops.”
The copyright is 2011 and I would love to know if there is updated information available on estrogen & breastfeeding. I like to stay up-to-date and wonder if I’m missing some new info. Is there a study that I can read? I’d greatly appreciate it!
Oh, and will definitely be buying the book–thanks!
I loved this episode! I am curious though about the fiber supplement for someone with gluten and wheat allergies. Will this cause a reaction by adding psyllium husk? Also, is there a brand or form you would recommend? Thanks for this awesome podcast! I look forward to Thursdays when a new one gets posted! 🙂
Hi, I loved this episode! Around 29:49 Dr. Gottfried mentions a supplement that she really likes and I can’t, for the life of me, figure out what she’s saying! I would love to look into it, so if you have the name of it that would be great, thank you!
Great podcasts with Dr. Gottfried, but a transcript would be helpful… I listen on my commute and can’t make notes. All the other ones have them – is there a reason these don’t?
This was just before we started having them done- it’ll get done in time.
Thanks!
This was just before we started having them done- it’ll get done in time.